Cluneal Nerve Entrapment
Lumbo-Pelvic Pain Part 2
 Maigne's Syndrome, Cluneal Nerve
Maigne's Syndrome, Cluneal Nerve
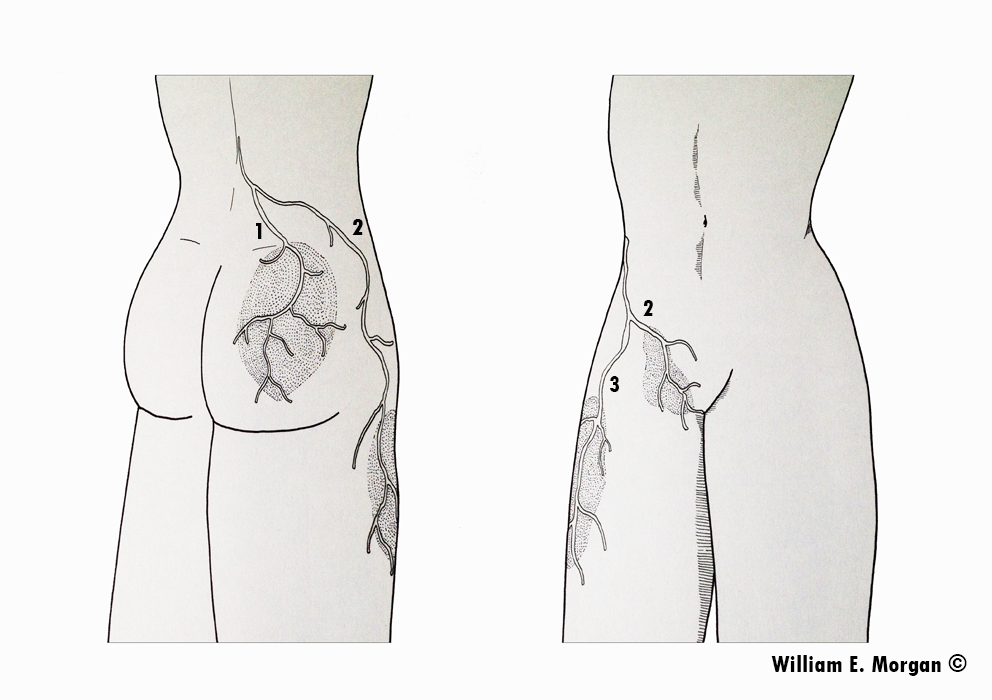
Figure 1. In the first article of this series I discussed Maigne’s syndrome (AKA thoracolumbar junction syndrome) as a potential source of lumbo-pelvic pain. This syndrome is identified by a triad pattern of pain involving the posterior pelvis, lateral thigh, and inguinal region. This image identifies the distribution of pain; (1) the posterior pelvis, (2) the inguinal region, and (3) the lateral thigh arising from dysfunction in the T10-L2 vertebral segments.
In the first article in this series we discussed the concept (initially described by the French physician Robert Maigne) of thoracolumbar facetal irritation creating symptoms in the posterior pelvis, the lateral thigh, and the inguinal region (figure 1). Maigne’s work explained that pelvic pain may originate higher in the trunk and arise from the lateral branches of the dorsal ramus. Maigne proposed that manipulation of the T10-L2 vertebral segments may reduce the symptoms associated with thoracolumbar junction syndrome. He uncovered this notion through research, clinical observation, knowledge of anatomy, and human dissection. While Maigne identified common pain distribution patterns, I should note that innervation from the lateral branches of the dorsal ramus may vary from person to person.
Superior Cluneal Nerve Entrapment
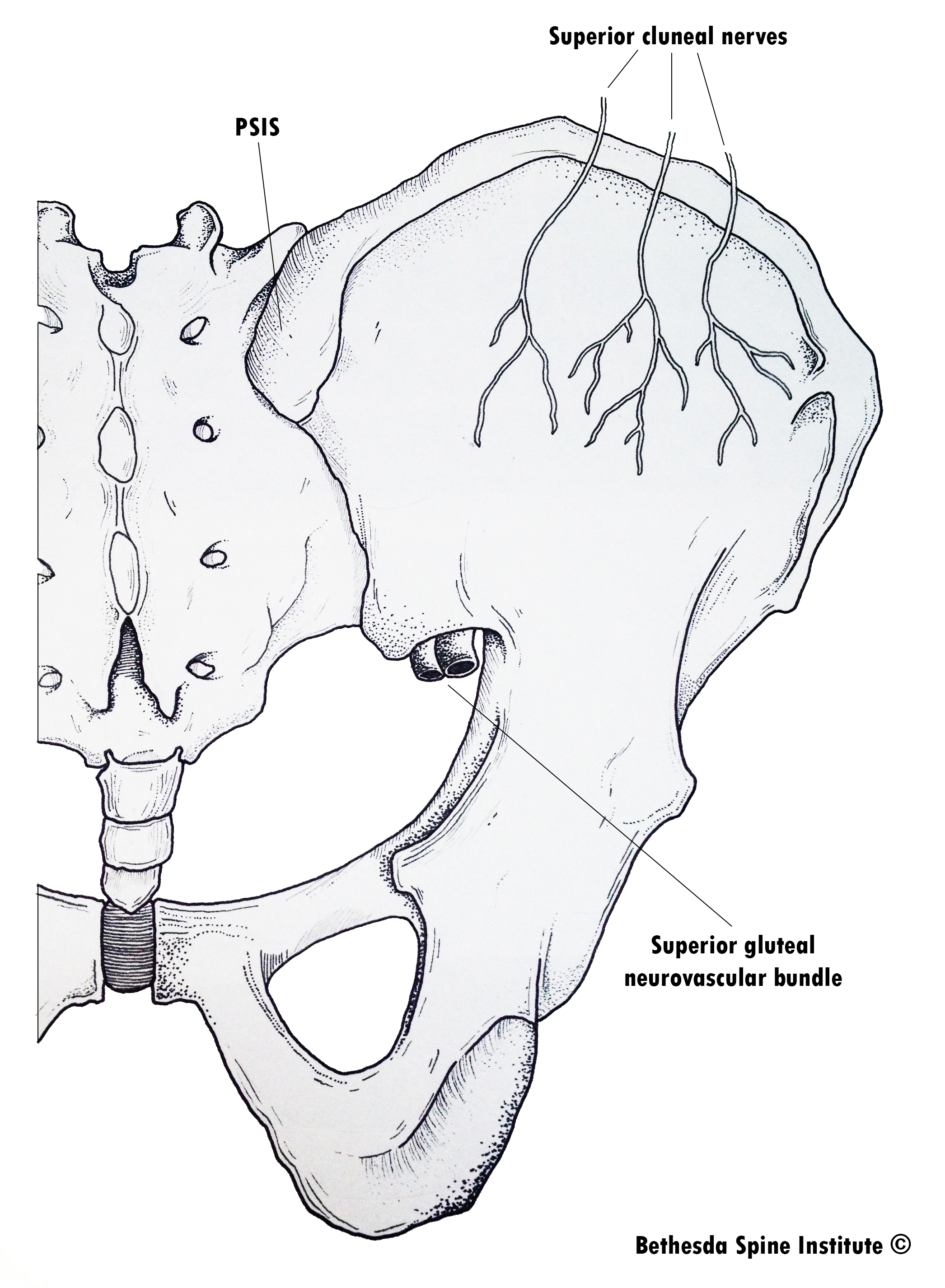
This article will focus on a peripheral nerve entrapment which may occur “downstream” from the thoraco-lumbar junction: superior cluneal nerve entrapment. Strong and Davila were the first to describe this condition in 1957. While the superior cluneal nerve neruopathy has been identified as a source of lower back and posterior pelvic pain, albeit rare, there has been little research on the effectiveness of treating this condition. The superior cluneal nerve originates from the posterior rami of L1-2-3, then descends inferior to cross over the crest of the ilium in three branches. The medial branch travels through an osteofibrous tunnel which has been cited as a site of entrapment similar to carpal tunnel syndrome. The osteo component of this tunnel is the rim iliac crest, and the fibrous component is composed of the tough thoracolumbar fascia.
Clinical Presentation of Superior Cluneal Nerve Entrapment
Superior cluneal nerve entrapment will present with pain over the posterior ilium and upper buttocks region. You may also feel a thickening of tissue along the rim of the posterior iliac crest, and there may be tenderness in this region. By tapping on the tender spot or thickened tissue, you may evoke a shock-like sensation. If this tapping produces an electrical shock-like sensation, it is considered a positive Tinel’s sign. This is strongly indicative of cluneal nerve involvement.
Treatment
Making the diagnosis of a superior cluneal nerve syndrome is easier than treating this disorder. Few inroads have been made studying the treatment of this malady, so we are left with mainly antidotal recommendations for treating pain attributed to the superior cluneal nerve entrapment. Medical practitioners may perform pain injection procedures or more rarely perform a surgical release of the entrapment.
Manual practitioners can utilize manipulation of the segments of innervation for this region (T11-L2), instrument assisted myofascial mobilization (such as Graston), pin and stretch techniques, and soft tissue mobilization techniques. While there is little evidence to validate this treatment as being effective in treatment of this condition, there is no evidence to indicate that it is not effective. Hence a trial treatment of manual methods is still prudent.
I treat superior cluneal nerve syndrome with adjustments and soft tissue mobilization using a motorized prone distraction table to elongate the fascia as I perform either a pin and stretch type “release” or use a myofascial mobilization instrument. While I feel that this technique is effective, it is based solely on antidotal experience. I would be the first to say research is needed to substantiate its effectiveness. While all healthcare professions use unsubstantiated treatment methods, we need to avoid making unsubstantiated claims about those treatments.
 Cluneal Nerve
Cluneal Nerve
Figure 2. The superior cluneal nerves cross over the rim of the iliac crest in three branches. While all branches may succumb to entrapment, the medial branch travels through an osteofibrous tunnel which makes it particularly susceptible to entrapment.
References
Tubbs RS, Levin MR, Loukas M, Potts EA, Cohen-Gadol AA: Anatomy and landmarks for the superior and middle cluneal nerves: application to posterior iliac crest harvest and entrapment syndromes. J Neurosurg Spine13:356–359, 2010.
Strong EK, Davila JC: The cluneal nerve syndrome; a distinct type of low back pain. Ind Med Surg 26:417–429, 1957.
Lu J, Ebraheim NA, Huntoon M, et al. Anatomic considerations of superior cluneal nerve at posterior iliac crest region. Clin Orth & Rel Res 1998;347:224-228.
Drury BJ. Clinical evaluation of back and leg pain due to irritation of the superior cluneal nerve. J Bone Joint Surg 1967;49A(1):199.
Maigne JY, Maigne R. Trigger point of the posterior iliac crest: painful iliolumbar ligament insertion or cutaneous dorsal ramus pain? An anatomic study. Arch Phys Med Rehabil 1991;72:734-737.
Maigne R. – Sémiologie des dérangements intervertèbraux mineurs. Ann. Med. Phys. 1972. 15, 277-289.
Kuniya H, et al. Prospective study of superior cluneal nerve disorder as a potential cause of low back pain and leg symptoms. Journal of Orthopaedic Surgery and Research (2014) 9:139.
