Don’t Shoot the Messenger…of Pain
Medial Branch Neurotomy
I am usually the one encouraging the cause of interdisciplinary collaboration. But there are times when I feel there are interventions that are inappropriately applied in medical pain practices. One that I am particularly skeptical about is a pain clinic procedure called a medial branch block or medial branch neurotomy. In this procedure the intent is to destroy the nerve (the medial branch of the posterior primary ramus) that innervates the facets in an attempt to treat back pain that originates in the facet.
Why is the Medial Branch Important?
This nerve is a key player in the reactive intersegmental stability and protection of the spine. The medial branch of the posterior primary ramus (division) innervates the zygapophyseal joints, interspinous ligaments, supraspinous ligament, ligamentum flavum, the periosteum of the vertebral arch, and the posterior spinous process. The medial branch also innervates (both motor and sensory) these muscles: multifidus, [i] intertransversarii, the rotatories, and the interspinous muscles.[ii]
All of these structures are part of a complex reactive mechanism that interacts to provide stabilization and protection to the spine. So when pain physicians treat facet pain with a neurotomy, they are also destroying the nerves to the spinal components that protect the facets from further damage.
Medial Branch Radiofrequency Neurotomy
Prior to performing a neurotomy, the pain physician usually performs a trial injection with anesthesia like lidocaine. The needle is guided with fluoroscopy. If the anesthesia reduces or eliminates the pain, that indicates to the physician that they have isolated the nerves that convey the sensation of pain to the facets. The physician will then use a radiofrequency ablation probe to produce enough heat to destroy the nerve. In time, the nerve may regenerate and the procedure may need to be repeated.
Denervation of the medial branch of the posterior primary ramus has demonstrated some potential for providing long term control of facet pain. While major harm caused by this procedure is very rare, the potential long term effect on the facets and other spinal anatomy (I guess this would be classified as minor harm) has not been adequately studied.
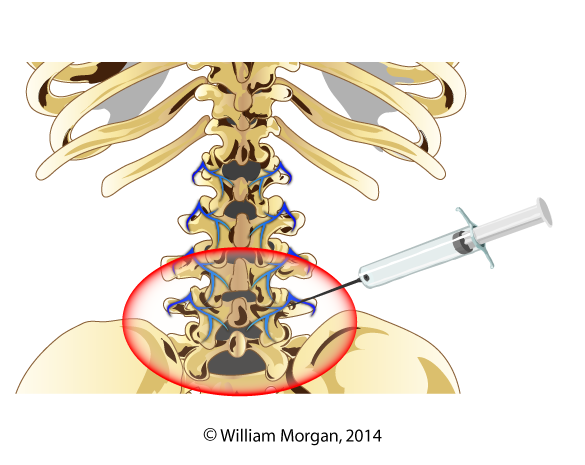 Medial Branch BlockMedial branch block with anesthesia
Medial Branch BlockMedial branch block with anesthesia
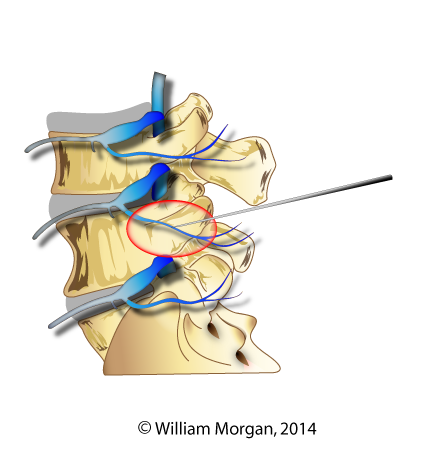 Neurotomy
Neurotomy
Radiofrequency neurotomy
Medical branch denervation procedures are being utilized on a grand scale without being substantiated by rigorous randomized controlled studies. In fact, one study that is highly referenced is a case series with only five patients! In this study, Dreyfus revealed that the multifidus did atrophy after radiofrequency neurotomy, but the authors concluded that this was inconsequential because of the pain relief that lasted for twelve months following the procedure. [iii] Multifidus atrophy of multiple levels following a single level medial branch radiofrequency ablation was identified through the use of electromyography in a case published by Wu.[iv] This shows diffuse atrophy of the multifidus muscles following radiofrequency ablation (RFA). A case series here and a case there may not seem like much to base so many conclusions on, but that is all we have. There is a deafening silence when it comes to researching the long term effects of this procedure on the zygapophoseal joints.
Something else that concerns me is the long term effects this procedure will have on the facets. Medial branch ablation effectively creates a Charcot joint of the facets. Charcot joint is the term given to a joint that has a neuroarthopathy that renders it devoid of sensation. The name Charcot’s joint was given by the French neurologist Jean-Marie Charcot who noted a pattern of joint destruction in patients with the loss of joint sensation. In a Charcot joint the patient is unable to perceive the pain of joint damage so they will engage in joint damaging activities and not even know it. Currently there are no randomized control studies we can look to that address the long term effects of spinal facet joint anesthesia.
Several years ago I was speaking at a foreign spine surgeon conference, the sole chiropractor speaking to hundreds of international spine surgeons. During a panel discussion I expressed my misgivings about neurotomy of the medial branch and its potential harm to the multifidus. One of the spine surgeons on the panel then proceeded to ridicule me in front of his colleagues and state that medial branch of the posterior primary rami is totally sensory; it does not have a motor component. I was dumbfounded. He is performing these procedures and did not even know that he was ablating a motor nerve.
I cornered the surgeon later in the conference and showed him the evidence that this nerve was indeed both motor and sensory. I was vindicated when, much to his credit, he acknowledged his mistake and apologized to me from the podium of the conference in front of the attendees.
From my experience and research I draw these conclusions: these procedures do reduce facet pain and can do it for a long time. These particular spinal procedures rarely cause life threatening harm. However, this procedure has risks for causing further harm to the facets and other structures of the spine and this procedure should only be performed after all other conservative care, including chiropractic, has failed. I also conclude that the long term effects of this procedure is understudied, and there is not nearly enough evidence for this procedure to be utilized at its current level.
[i] MacDonald DA, Moseley GL, Hodges PW. The lumbar multifidus: does the evidence support clinical beliefs? Man Ther 2006;11:254–63. Epub 2006 May 23
[ii] Cramer G, Darby S (2013). Basic and clinical anatomy of the spine, spinal cord, and ANS (third edition). Elsevier Mosby. Page 303
[iii] Dreyfuss P, Stout A, Aprill C, et al. The significance of multifidus atrophy after successful radiofrequeny neurotomy for low back pain. PM R 2009;1:719–22
[iv] Wu PB, Date ES, Kingery ES. The lumbar multifidus muscle in polysegmentally innervated. Electromyogr Clin Neurophysiol 2000;40:483–85
