Gluteal Activation Enhances Athleticism and Injury Prevention
By Chris Feil, DC and William E. Morgan, DC
Editor's note: This is the fourth in a continuing series on cross-fitness training. The first article appeared in the Sept. 9, 2009 issue; the second in the Oct. 7, 2009 issue; and the third in the Nov. 4, 2009 issue.
For most athletes, success is largely dependent on optimal functioning of the gluteal muscles (gluteus maximus, medius and minimus), and functional integrity of the hips and pelvis. Unfortunately, functional training and evaluation is not well-understood by many practitioners and athletes. Appropriate gluteal activation and pelvic-hip control is not only important to the rising number of cross-fitness devotees for generating maximal athletic power; it is also important to virtually every chiropractic patient. In addition to generating athletic power, proper hip function is valuable in the prevention of injuries to the knees, hips, pelvis and lower back. The cross-fitness activities of squatting, cleans, kettlebell swings, tire flipping, medicine ball tossing, and sprinting are all multi-joint movements that require hip involvement. Let's discuss methods to maximize proper hip motion and form during these activities.
Many in modern society have what Stuart McGill, PhD, calls "gluteal amnesia."1 Dr. McGill has identified that when athletes [or any of us] lose the ability to engage our hips during athletic activities or exercises (such as cross-fitness programs), this adversely affects performance and increases the likelihood of injury. What Dr. McGill calls "gluteal amnesia," we might identify as loss of functional hip integrity: essentially the loss of the normal volitional ability to move one's hips through their range of motion with appropriate muscle activation.
In addition to muscular inhibitions, other factors that may contribute to motion dysfunctions are soft-tissue contractures or restrictions and articular fixations. While chiropractic adjustments may directly affect these restrictive lesions, knowledge of gluteal activation is also required to teach patients how to properly activate these muscles.
Function of the Gluteus Maximus
The gluteus maximus (GM) is the largest muscle of the body, and it is the major driver in lifting, throwing, swinging, pushing and running (particularly when sprinting and running hills). The GM originates at the crest of the pelvis, the dorsal sacral ligament, along with some fibers that originate from the thoracodorsal fascia. The [distal] insertions attach to the femur and to the iliotibial band. The GM helps stabilize the sacroiliac (SI) joints by causing force closure, essentially forming a self-bracing, protective compressive force to maintain the alignment and reduce shear forces on the SI joint. The GM attachment to the sacral ligaments may aid in pelvic stability due to active ligament tightening by gluteal contraction.2
The late professor Vladimir Janda associated decreased GM control in his theory of lower cross syndrome.3-4 This muscle imbalance is associated with the pelvic posture variation called anterior pelvic tilt. Observing anterior pelvic tilt during a postural examination of a patient should provoke you to further screen for gluteal dysfunction.
The gluteal muscles are the primary extensors of the hip, but hip extension is only part of their role in true athletic function. The muscle fibers of the GM are oriented diagonally, sloping laterally and caudally from their origin. With this orientation, the GM muscles contribute to external rotation and abduction of the thigh. Both hip extension and thigh external rotation are the "concentric" motions of the GM muscle.
It is important to remember that muscles have two contractile functions: concentric contractions (muscle shortening) and eccentric contractions (muscle lengthening). Eccentric muscle contraction is actually more powerful and more efficient than concentric contractions. The eccentric function of the GM muscle will limit and control hip flexion and thigh internal rotation.
Because of its fiber orientation, the GM serves as a primary muscular shock absorber for the hip and knee joint. Just as the hydraulic shock compresses and dampens the load in a car, the GM dissipates the forces in the athletic movements of jumping, landing, and lateral agility motions by eccentrically absorbing forces and limiting movements endangering joints of the lower extremities.5 The link between GM dysfunction and uncontrolled valgus and internal rotation motions of the knee has particular clinical significance and will be discussed in greater detail in an upcoming article.
Tremendous loads can be transmitted through the acetabulofemoral joint if the force is not dampened by the adjacent muscles. This shock absorption function is important to understand in a culture in which so many degenerative hip disorders occur. As many desk-bound workers with inadequate GM control participate in cross-fitness programs, they are unknowingly placing themselves at greater risk for osteoarthritis in their hips.
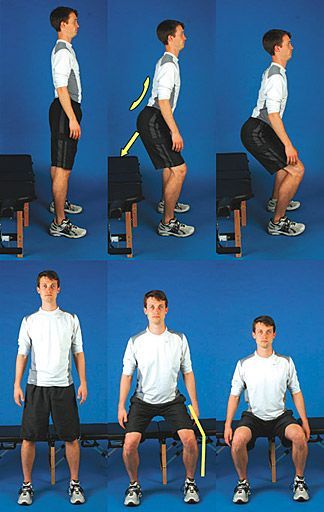 Figure 1: Squat Functional Screen: Passing. Normal lumbar lordosis, posterior travel of hips, varus knee position, and limited anterior travel of knees. Initiating Movement at the Hip and GM Activation
Figure 1: Squat Functional Screen: Passing. Normal lumbar lordosis, posterior travel of hips, varus knee position, and limited anterior travel of knees. Initiating Movement at the Hip and GM Activation
Elite power-lifters are able to squat more than 1,000 lbs injury-free through very purposeful activation of the GM and maximizing hip motion with the hip hinge.6 The term hip hinge refers to truncal motion in which the lumbar spine is fixed in a neutral lordosis and all motion occurs at the acetabular joint, not the spine.
An ideal squat begins by securing the toes and heels firmly on the floor. The lumbar spine should be fixed or "locked" into a neutral lordosis throughout the squatting motion. While descending, the buttocks should travel back and down; using a stool, gym ball, or chair as a target may be beneficial in learning this motion pattern. A wide stance is preferred, and the participant should be mindful not to allow the knees to travel forward.
Purposely engage the GM throughout the squatting motion both during decent and ascent; the use of an elastic exercise band around the thighs will help the patient to consciously engage the GM. The ascent phase of a squat reverses the motion groove of the descent phase. It should also be noted that the patient needs to stiffen the core during hip hinges and squatting
The Squat as a Functional Screen for Gluteal Activation
Inspecting a patient's ability to squat is a practical method for clinical screening of the lumbo-pelvic-femur chain. While the patient performs repetitive squatting motions, analyze the three main components of gluteal involvement: hip extension, flexion and external rotation.
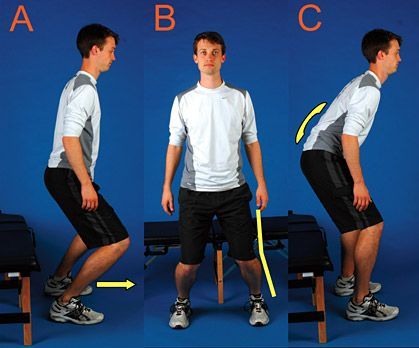
Figure 2: Squat Functional Screen - Failures. Anterior knee travel, valgus knee position, and loss of lumbar lordosis.
A key point in assessment is the initiation of hip movement before knee flexion or ankle dorsiflexion. The knee should remain in a varus position throughout the squatting motion. The lumbar lordosis should remain unchanged during the entire squat. (Figure 1) Early anterior knee translation (Figure 2a), a valgus knee angle (Figure 2b), and a flexed lumbar spine (Figure 2c) are failures for the squat functional screen.
 Figure 3: Squat Functional Screen - Palpation. The clinician provides challenge by applying medially directed pressure on the knees while the patient performs a squat. The examiner should palpate the GM for activation throughout the movement of both ascending and descending phases of the squat. In addition to palpating the GM, activation of the gluteus maximus can be tested by applying medial pressure to the knees. If the GM is engaged the examiner will note springy, firm resistance. With proper GM function, it should be difficult for the examiner to push the squatter's knee into a valgus position. (Figure 3) With practice and patience, you will be able to identify motion defects and provide precise recommendations for improving motion patterns.
Figure 3: Squat Functional Screen - Palpation. The clinician provides challenge by applying medially directed pressure on the knees while the patient performs a squat. The examiner should palpate the GM for activation throughout the movement of both ascending and descending phases of the squat. In addition to palpating the GM, activation of the gluteus maximus can be tested by applying medial pressure to the knees. If the GM is engaged the examiner will note springy, firm resistance. With proper GM function, it should be difficult for the examiner to push the squatter's knee into a valgus position. (Figure 3) With practice and patience, you will be able to identify motion defects and provide precise recommendations for improving motion patterns.
Athletes performing cross-fitness feats of strength, agility, and endurance with functional impairments can expect to have reduced levels of performance and increased occurrences of injury and infirmity. Gluteal activation and properly functioning hip mechanics are fundamental components of proper motion and maximized athletic performance. Cross-fitness devotees with impaired gluteal/hip function can expect diminished performances and increased risk of injury. An astute clinician should be able to observe a cross-fitness athlete's squat and discern gluteal function and activity, correcting those at risk before injury occurs.
References
- McGill S. Low Lack Disorders: Evidence-Based Prevention and Rehabilitation, 2nd Edition. Champaign: Human Kinetics, 2007:110-112.
- Wilson J, et al. A structured review of the role of gluteus maximus in rehabilitation. New Zealand Journal of Physiotherapy, 2005;33(3):95-100.
- Bullock-Saxton JE, Janda V, Bullock MI. Reflex activation of gluteal muscles in walking. Spine, 1993;18(6):704-8.
- Morris CE, Chaitow L, Janda V. Functional Examination for Low Back Syndromes. In: Morris C. Low Back Syndromes: Integrated Clinical Management. McGraw-Hill, 2006:347.
- Boling MC, Padua DA, Creighton RA. Concentric and eccentric torque of the hip musculature in individuals with and without patellofemoral pain. Journal of Athletic Training, 2009;44(1):7-13.
- Liebenson C. The hip hinge. Journal of Bodywork and Movement Therapies, 2003;7:151-152.
The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense or the U.S. government.
This is a reprint from Dynamic Chiropractic – January 29, 2010, Vol. 28, Issue 03
