By Chris Feil, DC and William E. Morgan, DC
As discussed in previous articles in this series, cross-fitness programs tend to advocate exercises that require maximal shoulder end-range motions: pull-ups (often with a kip or a jerk motion at end range), handstand presses, press squats, push-presses, clean and presses, kettlebell overhead lifting, gymnastic ring work and other similar exercises.
To perform these motions without injury requires unfettered shoulder range of motion and optimum shoulder stability. While an argument may be made that these exercises help to create coordinated athletic patterns of strength, agility, and stamina, they still have a strong potential for causing shoulder injuries. Often not included in the explanation of the workout of the day in cross-fitness programs is the need for the participant to have flawless shoulder mechanics and strength.
Impingement of the rotator cuff muscle (supraspinatus) develops when the space between the rigid coracoacromial arch and the head of the humerus narrows. The muscles and tendons of the cuff that pass through this space begin to fray and eventually may tear because they are pinched between these hard surfaces. Why does this space narrow? Anatomically, it narrows due to bony spurs, degenerative changes, or soft-tissue thickening. Functionally, the space narrows due to dysfunctional synchronicity of the rotator cuff muscles, aberrant scapular-humeral rhythm, or faulty scapular positioning during overhead arm movements.
To maintain the subacromial space in an overhead arm movement, the scapula must retract and tilt posterior.7 A shortened pectoralis minor will cause the scapula to tilt anterior, contributing to a functional shoulder impingement. A study conducted at Ohio State University found that subjects with tight and short pectoralis minor muscles displayed similar scapular kinematics as individuals with shoulder impingements.1 Scapular retraction is affected by the mobility of the thoracic spine and rib cage upon which it glides.9
Thoracic Spine Mechanics and Shoulder Pain
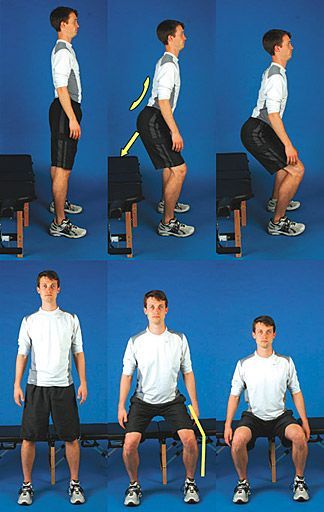
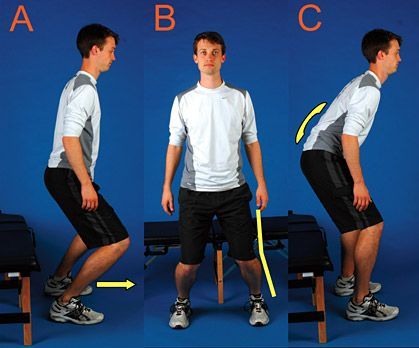
 Normal scapular and thoracic spine motion allows optimal mechanics for athletic shoulder motions (left). Increased thoracic kyphosis, reduced thoracic mobility, or scapular protraction from pectoralis minor tautness can contribute to shoulder impairment and injury (right). The concept of scapulo-humeral rhythm is well-documented,4,7 and the rhythm is fundamental to maintaining the subacromial space. The long-accepted linear ratio of scapular rotation to arm motion in adduction is 1:2,2 though the true interaction of the scapula and arm is not linear, but more curvilinear in nature.8 There is very little scapular rotation in the first 60 degrees of arm abduction, and then the scapula progressively begins to rotate as the arm travels to a full overhead position.4
Normal scapular and thoracic spine motion allows optimal mechanics for athletic shoulder motions (left). Increased thoracic kyphosis, reduced thoracic mobility, or scapular protraction from pectoralis minor tautness can contribute to shoulder impairment and injury (right). The concept of scapulo-humeral rhythm is well-documented,4,7 and the rhythm is fundamental to maintaining the subacromial space. The long-accepted linear ratio of scapular rotation to arm motion in adduction is 1:2,2 though the true interaction of the scapula and arm is not linear, but more curvilinear in nature.8 There is very little scapular rotation in the first 60 degrees of arm abduction, and then the scapula progressively begins to rotate as the arm travels to a full overhead position.4
Normal thoracic-humeral rhythm is important for injury prevention. Thoracic mobility becomes increasingly important in athletic overhead activities. The higher an athlete raises their arm, the more thoracic motion is needed from the thoracic spine to maintain the proper relative shoulder alignment. Individuals with a shoulder impingement have statistically less thoracic mobility and a more kyphotic thoracic spinal posture than individuals with healthy shoulders.3,6-7 A few weeks of cross-fitness training with a rigid thoracic spine could lead to injury and impairment of the rotator cuff.
Does T4 Syndrome Exist?
T4 syndrome has been accepted as fact by many clinicians over the past decade, in spite of a lack of evidence to support its existence. The theory of T4 syndrome attributes many of the problems seen in shoulders to a loss in the normal extension that takes place at the T4 vertebra.5 We should note that T4 syndrome has also been credited with causing diffuse arm, shoulder, and torso pain and sensory symptoms.
A review of the literature review did not find research substantiating association of the T4 syndrome to shoulder function. However, we did find a boatload of seminar notes elevating the "T4 syndrome" to a height not supported by the current body of research. T4 syndrome is based on clinical antidotal experience rather than scientific evidence. While there is no substantial evidence that T4 syndrome directly relates to shoulder impingement, there is some current research pointing to the lower thoracic spine as being a fundamental component of shoulder motion.4
If accurate, this research suggests that the majority of thoracic extension occurs in the lower thoracic spine during overhead arm movement in asymptomatic shoulders, especially with both arms in an elevated position, as is seen in an overhead squat or overhead press.
In the same study, upper thoracic extension was present in full overhead arm motion, but it was not deemed to be a significant variable in shoulder function.4 However, what the study did find statistically significant in the upper thoracic spine was lateral bending and ipsilateral rotation during single-arm elevation. Theodoridis and Ruston also found this repeatable relationship of overhead arm movement causing an ipsilateral coupling pattern between lateral flexion and rotation, which was repeatable and comparable for both arm elevation planes in healthy subjects.11
Thoracic Joint Manipulation
It appears that simply assessing T4 extension in a cross-fitness athlete may miss significant dysfunctions in the thoracic spine that affect the thoracic-humeral rhythm. For example, optimal shoulder function in a single-arm kettelbell swing may be improved by use of manual therapy when specifically addressing lateral bend and rotation components of the upper thoracic spine and any loss of extension in the lower mid-thoracic spine.
Thoracic joint manipulation might be the simplest answer to reducing pain in an impinged shoulder. In a 2009 study by Strunce and colleagues, a thoracic spinal manipulative thrust was performed on a sample of 56 individuals with symptomatic shoulders from impingement. After two days, there was a significant decrease in pain levels in over 50 percent of individuals.10
Before giving a list of boring rotator-cuff strengthening exercises to a cross-fitness athlete who is performing fun, dynamic exercises in their daily workouts, remember that a key component to overhead arm motion is thoracic mobility. When the alignment of the shoulder and the subacromial space is compromised from the loss of thoracic spine mobility and/or muscle tightness, it doesn't matter what tension of rehab exercise band is used until the underlying cause of impingement is addressed. Evaluation and appropriate treatment of the spine should be considered when shoulder dysfunction is present.
The cross-fitness emphasis on pull-ups and overhead lifting may produce a glut of shoulder injuries from otherwise dormant thoracic and shoulder impairments. By recognizing the functional relationship between the thoracic spine and the shoulder joints, we can help athletes remain active and pain-free as they engage in their preferred activities.
References
- Borstad JD, Ludewig PM. The effect of long versus short pectoralis minor resting length on scapular kinematics in healthy individuals. Journal of Orthopedic Sports Physical Therapy, 2005;4:227-238.
- Codman EA. The Shoulder; Rupture of the Supraspinatus Tendon and Other Lesions in or About the Subacromial Bursa. Thomas Todd, Boston, 1934.
- Crawford HJ, Jull GA. The influence of thoracic posture and movement on range of arm elevation. Physiotherapy Theory and Practice, 1993;9:143-148.
- Crosbie J, Kilbreath SL, Hollmann L, York S. Scapulohumeral rhythm and associated spinal motion. Clinical Biomechanics, 2008;23:184-192.
- DeFranca GG, Levine LJ. The T4 syndrome. Journal of Manipulative and Physiological Therapeutics, 1995;1:34-37.
- Greenfield B, et al. Posture in patients with shoulder overuse injuries and healthy individuals. Journal of Orthopedic Sports Physical Therapy, 1995;5:287-295.
- Kibler BW. The role of the scapula in athletic shoulder function. The American Journal of Sports Medicine, 1998;26:325-337.
- McClure PW, Michener LA, Sennett BJ, Karduna AR. Direct 3-dimensional measurement of scapular kinematics during dynamic movements in vivo. Journal of Shoulder and Elbow Surgery, 2001;10:269-277.
- Stewart S, Jull GA, Ng, JKF, Willems JM. An initial analysis of thoracic spine movement during unilateral arm elevation. Journal of Manual & Manipulative Therapy, 1995;3:15-20.
- Strunce J, et al. The immediate effects of thoracic spine and rib manipulation on subjects with primary complaints of shoulder pain. Journal of Manual & Manipulative Therapy, 2009;17:230-236.
- Theodoridis D, Ruston S. The effect of shoulder movements on thoracic spine 3D motion. Clinical Biomechanics, 2002;17:418-421.
The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense or the U.S. government. This is the fourth in a continuing series on cross-fitness training. The first article appeared in the Sept. 9, 2009 issue; the second in the Oct. 7, 2009 issue; the third in the Nov. 4, 2009 issue; and the fourth in the Jan. 29, 2010 issue.
Reprinted from Dynamic Chiropractic – May 6, 2010, Vol. 28, Issue 10