Arachnoiditis
Incurable, disabling, controversial and heading your way
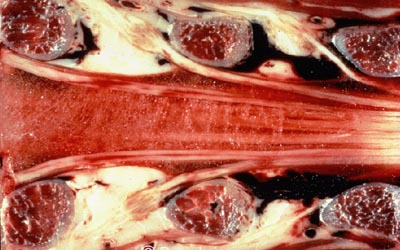
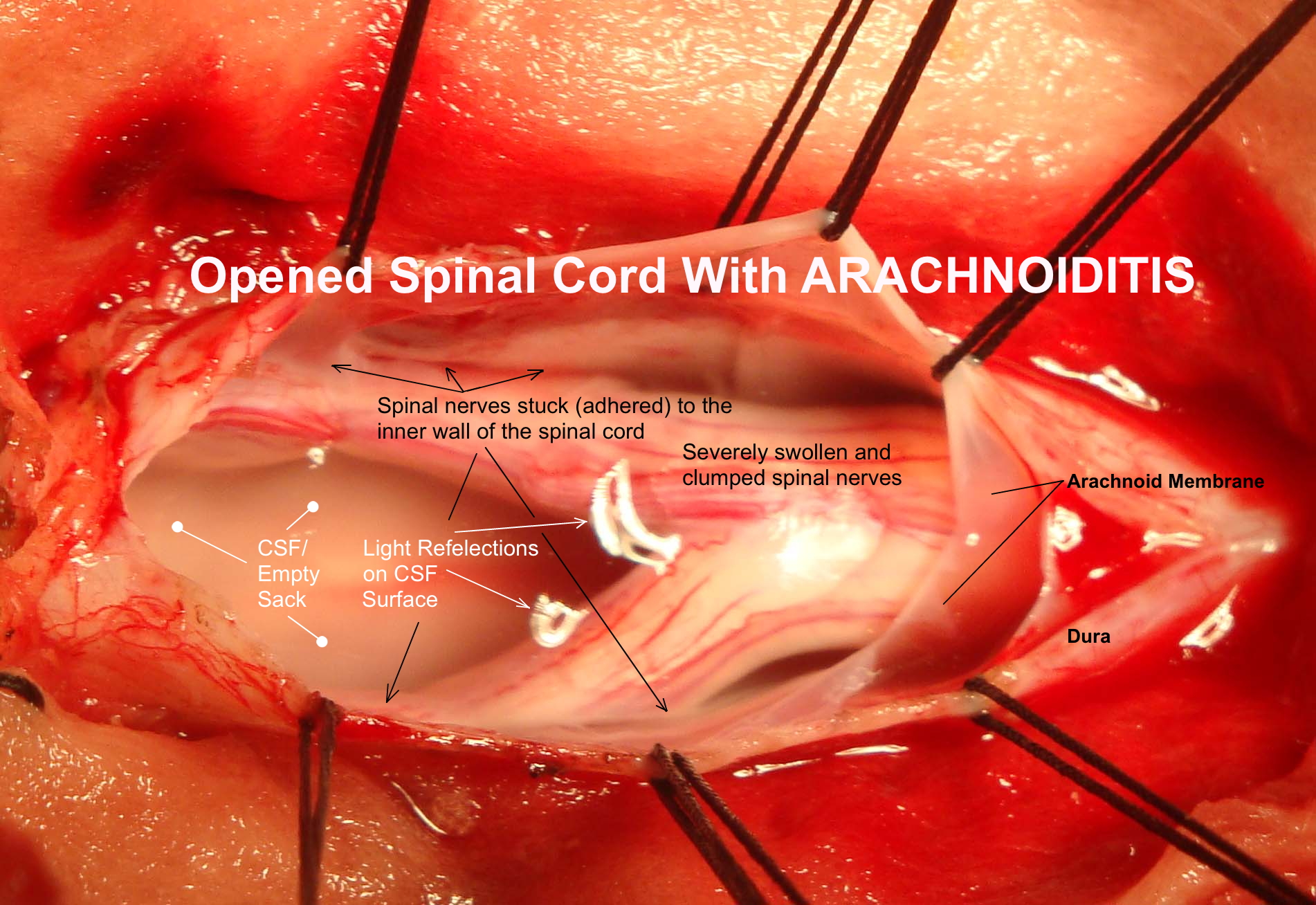
Misunderstood and underreported, arachnoiditis can result from routine medical procedures and leave patients permanently incapacitated. Arachnoiditis is a neuropathic malady that affects the arachnoid layer of the meninges. A more severe type of arachnoiditis is adhesive arachnoiditis. Adhesive arachnoiditis results in scarring and adhesions within the meninges. Additionally, it compresses the nerve rootlets within the thecal sac and can cause nerves to adhere to one another. While described as a rare condition, it has become evident to me that there is no clear tracking method for this disease and that many cases may go undiagnosed. Since many doctors are not familiar with this condition, it may be mistaken for other conditions such as disc extrusions, cauda equina syndrome, failed back surgery, or multiple sclerosis.
Refractory pain is the predominant symptom of arachnoiditis. Other symptoms include urinary and bowel dysfunction, sexual dysfunction, numbness, tingling, loss of mobility, headaches, fatigue, and extremity pain and weakness. Since there is no consistent pattern of symptoms for this malady, a correct diagnosis maybe difficult.
Treatment of arachnoiditis is difficult and frequently focused on pain reduction. Spinal procedures (epidural injections, intrathecal injections, and surgery) may cause or worsen this condition so they are typically avoided. Medical management is often limited to protracted use of opiates, antidepressants, steroids, and other treatments intended to minimize pain. Since the degree of symptoms may vary in severity, some patients with arachnoiditis may live relatively normal lives and can be managed with interdisciplinary care: medical care, chiropractic, psychology and physical therapy. While none of these professions can claim to cure or even help every case of arachnoiditis, any treatment that is safe and may control the symptoms should be considered.
Causes
Three causes have been identified to induce arachnoiditis: Chemicals, trauma, and infection.
Ironically most cases of arachnoiditis are attributed to iatrogenic causes. The chemicals used in spinal injections are the leading iatrogenic cause of this condition. The trauma of a lumbar puncture, spinal surgery, and injury can also cause arachnoiditis. The chronic trauma of spinal stenosis, and disc derangement has also been cited to cause arachnoiditis.
Infection is another cause of arachnoiditis. Meningitis (viral, fungal, or bacterial) can result in arachnoiditis. The one case of infectious arachnoiditis that I have knowingly encountered was caused by tertiary Lyme disease.
Radiographic findings
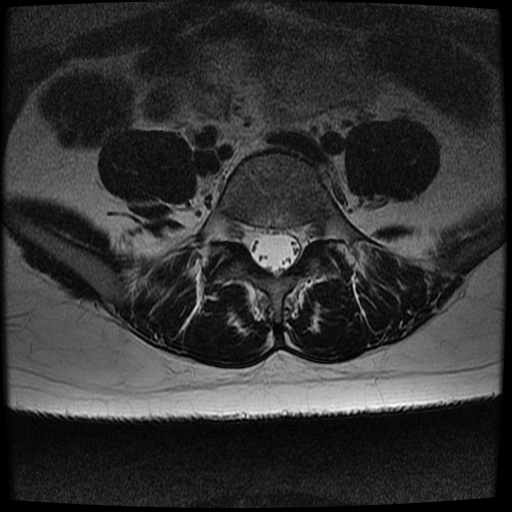
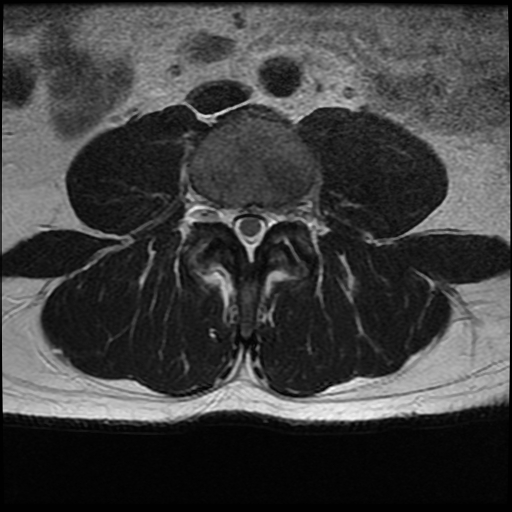
While plain film radiographs will not contribute to the diagnosis of arachnoiditis, magnetic resonance images can reveal characteristic findings of arachnoiditis. On MRI, compression or adhesion of nerve rootlets of the cauda equina may be visualized. The nerve rootlets of cauda equina will frequently be clumped in the anterior portion of the thecal sac in patients with adhesive arachnoiditis rather than in their normal location which is more posterior.
Conclusion
As epidural steroid injections and percutaneous spinal procedures become more routine and widely used, we can expect to see a rising number of these patients entering our offices.
Chiropractors and all spine practitioners should be familiar with this condition and its effects, realizing that we will not be able to cure patients with this malady. We may participate in the multidisciplinary management of these patients. Like many chronic pain syndromes an integrated team approach is preferred.