Building a Culture of Continuous Improvement
Self-Evaluation of Practice Performance
In institutional healthcare there is a requirement of continual self-reflection and improvement. Any chiropractor who has integrated into an institutional healthcare facility is probably already familiar with the term P.E. & I. –Performance (or Process) Evaluation and Improvement. Accrediting bodies in mainstream healthcare require ongoing projects that include self-reflection, analysis and improvement for hospitals and medical centers. In fact some medical societies and organizations are also implementing P.E. & I. as a requisite to certification.
If you are entering into integration with an institutional health care faculty (hospital-based, university-based, military, VA, public health service clinic…) you should be familiar with this method of continual analysis and improvement. In fact, even if you are not involved in an organization that requires ongoing P.E. & I. projects, it is a virtuous discipline to incorporate into your practice.
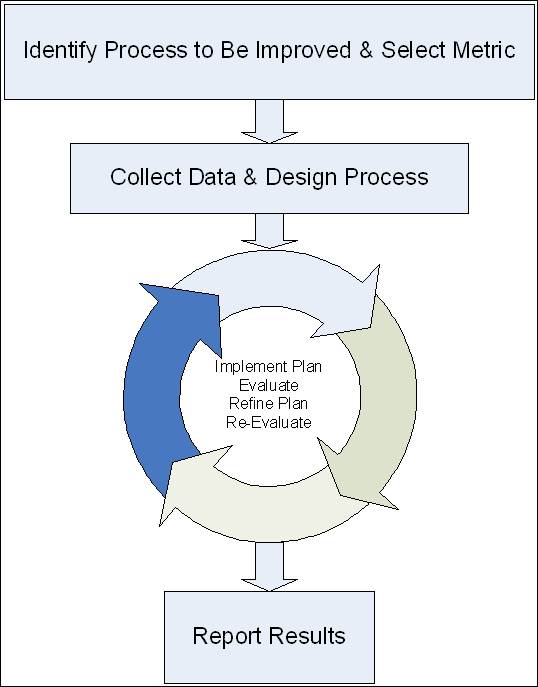
The concept is simple: Identify an area in your clinic that needs improvement, select a metric (unit of measurement), measure existing trends using this metric, implement a program of improvement, re-measure metric, modify program as required to maximize your improvement.
Some medical specialties, such as the American Board of Internal Medicine, have created kits for practice evaluation and improvement. A physician completing these projects can even receive CE credits.
An Example of Performance Evaluation and Improvement in Action
Selecting the Process to be Improved and the Measurement Metric
A doctor is concerned about her utilization of outcome measurement tools in her clinical practice. For her metric she decides to measure the number of lower back pain patients completing Roland-Morris questionnaires.
Collecting Initial Data
The doctor has her staff randomly survey 100 patient charts and finds out that 30 % of her patients with lower back pain have completed these surveys on their initial visits, and 5% complete follow-up questionnaires.
Designing and Implementing a Corrective Plan
She selects a plan that empowers her staff to have all new lower back pain patients complete a Roland-Morris at the time of their first visit. The staff then is allowed creative license to create a system that ensures that these patients continue to complete these forms every two weeks until case completion.
Evaluation and Tweaking the Plan
A few months later the staff performs another random chart survey and discovers that they now have 60% completion of the form on initial presentation and 50 % of these patients have completed follow-up questionnaires. After some analysis the doctor identifies a flaw in her plan: she failed to account for established patients coming in for new lower back injuries. She “tweaks” her plan and continues the process. During ensuing months she makes minor modifications to her plan until a successful outcome is obtained. If she worked in a monitored facility, she then completes a report on this project.
The Goals of Practice Performance Projects
The short-term goal of these self-reflective projects is to introduce doctors to the competencies of practice-based learning and information systems.
The long-term goal for these required competencies is to produce doctors who are proficient in understanding and using informatics, science-based practice improvements, and systems-based practice tools. Chiropractors seeking collaborative relationships with larger institutions will need to be able to demonstrate their adherence to high levels of accountability and professional values as well as maintaining a culture of continual reflection and improvement.
 PE & I
PE & I
